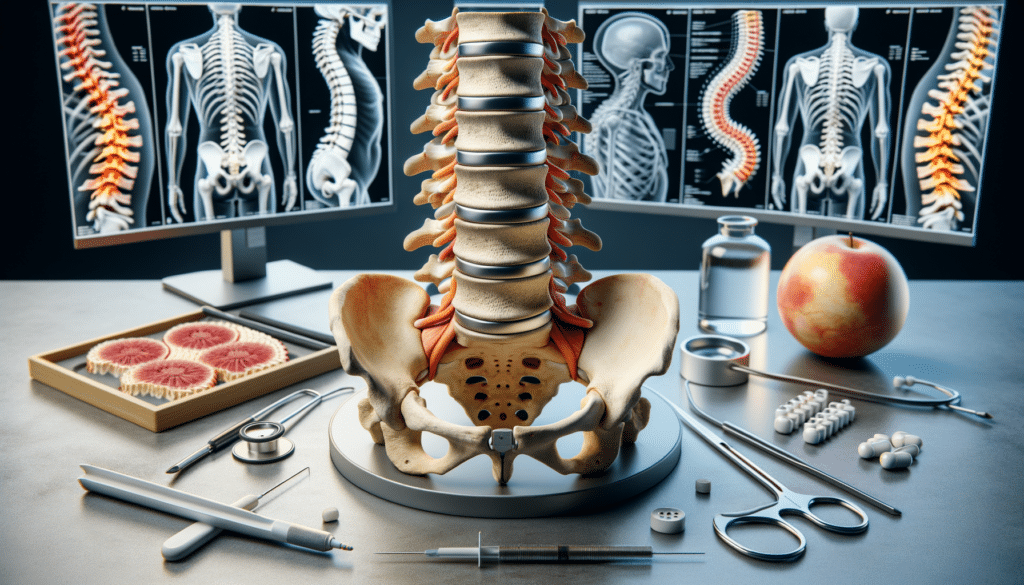
Understanding Spinal Stenosis: Causes and Symptoms
Spinal stenosis occurs when the spaces within the spine narrow, putting pressure on the nerves that travel through the spine. This condition can lead to a range of symptoms, from mild discomfort to severe pain. The most common causes of spinal stenosis include age-related changes, such as osteoarthritis and the thickening of ligaments. Other contributing factors may include spinal injuries, tumors, or congenital conditions affecting the spine. Symptoms often vary depending on the location of the stenosis but typically include pain, numbness, muscle weakness, and impaired balance.
Understanding the underlying causes and symptoms of spinal stenosis is crucial for effective management. Patients often experience a gradual onset of symptoms, which may worsen over time. In some cases, individuals may find relief through specific postures or movements, such as bending forward or sitting, which can temporarily alleviate nerve pressure. Early diagnosis and intervention are key to preventing the progression of symptoms and improving quality of life.
Non-Surgical Treatments for Spinal Stenosis
Non-surgical treatments are often the first line of defense in managing spinal stenosis. These therapies aim to relieve symptoms and improve function without the need for invasive procedures. Physical therapy plays a pivotal role in this approach, focusing on exercises that strengthen the muscles supporting the spine, improve flexibility, and enhance balance. A tailored physical therapy program can significantly reduce pain and improve mobility.
In addition to physical therapy, medications such as nonsteroidal anti-inflammatory drugs (NSAIDs) can help manage pain and inflammation. Epidural steroid injections are another option, delivering corticosteroids directly into the spinal canal to reduce inflammation and alleviate pain. While these injections do not cure spinal stenosis, they can provide temporary relief and improve the patient’s ability to participate in physical therapy.
Other non-surgical treatments include lifestyle modifications, such as weight management and activity modification, to reduce stress on the spine. Assistive devices, like braces or canes, may also be recommended to improve stability and mobility. These conservative treatments can be highly effective for many individuals, allowing them to maintain an active lifestyle without surgery.
When Surgery Becomes Necessary: Surgical Options for Spinal Stenosis
While non-surgical treatments can be effective for many, some individuals may require surgical intervention to achieve relief from spinal stenosis. Surgery is typically considered when conservative treatments fail to alleviate symptoms or when neurological deficits, such as significant weakness or loss of bladder control, occur. The goal of surgery is to decompress the affected nerves and stabilize the spine.
Several surgical options are available, each tailored to the patient’s specific condition and needs. Laminectomy, one of the most common procedures, involves removing part of the vertebra to relieve pressure on the spinal cord and nerves. Foraminotomy is another option, focusing on widening the foramina, the openings through which nerve roots exit the spine. In some cases, spinal fusion may be performed to stabilize the spine after decompression surgery.
Advancements in surgical techniques, including minimally invasive procedures, have improved outcomes and reduced recovery times. These techniques involve smaller incisions and less disruption to surrounding tissues, leading to faster healing and reduced postoperative pain. However, surgery is not without risks, and patients should thoroughly discuss potential benefits and complications with their healthcare provider to make an informed decision.